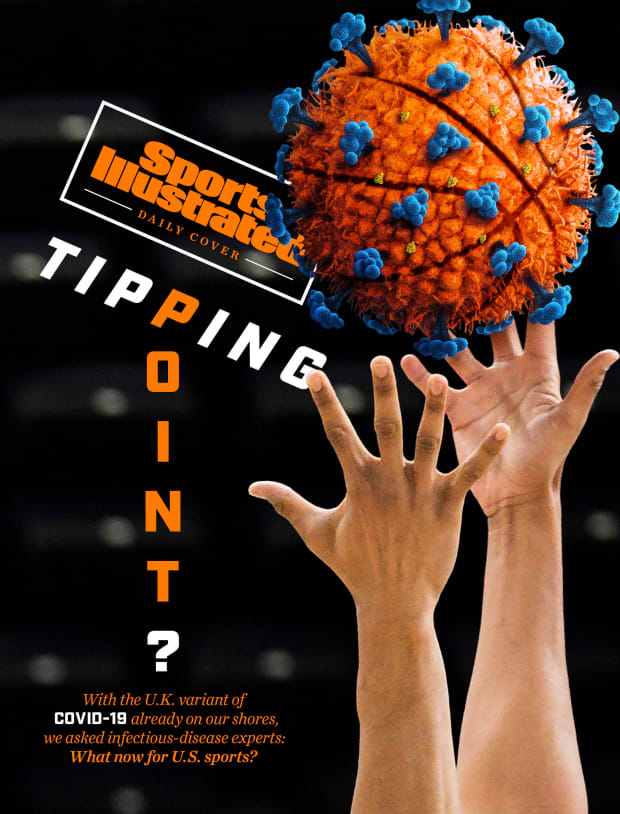
As the U.K. wonders whether it's again time to stop playing, SI polled infectious disease experts for a little coaching on what comes next.
As a professor of infectious-disease epidemiology at the London School of Hygiene and Tropical Medicine, Adam Kucharski has been far too busy in recent weeks to watch much Premier League action. “I was working, unfortunately,” he says. Then again, as a soccer fan in England, he hasn’t been able to escape the drama enveloping his favorite game.
Earlier this month, even as the U.K. entered its third lockdown of the pandemic, government officials granted special dispensation for “elite” pro sports to continue. The results have not been pretty, particularly on the pitch: A half-dozen Premier League players drew rebukes from their clubs for attending holiday parties. Viral videos showed crowded locker rooms, with unmasked celebrants belting out full-throated songs. One COVID-19 outbreak forced Aston Villa to play Liverpool with a roster of U-23 and U-18 prospects, many of whom had been dropped off by their parents, seeing as they were too young to drive.
Against a backdrop of surging cases and deaths, in large part due to a new, highly transmissible variant of COVID-19, these bad-look incidents have prompted thorny questions across the pond. “There have obviously been the bubble systems with the NBA and other leagues—and in some cases that’s been very successful,” says Kucharski. “But that becomes harder with larger amounts of community transmission. So those questions are cropping up: What activities do we want to prioritize? … And I think some countries will soon have to make some very hard decisions about what to keep open.”
In the U.S., it was hoped that these issues were left behind last summer, when leagues emerged from early-pandemic hibernation to resume playing in so-called bubbles; instead, like the virus itself, they have been growing in force of late. After failed tests, the Browns lost two cornerbacks and their coach, Kevin Stefanski, for a playoff game; the Packers lost an offensive lineman. The NBA, facing decimated rosters, postponed 13 games between Jan. 10 and Jan. 18. And in the NHL, the reigning Western Conference–champion Stars suffered an outbreak of 17 infected skaters at training camp.
As bad as that may seem, the U.K. offers a sobering look at what could soon be coming stateside. In particular, the rapid worldwide emergence of several über-contagious COVID-19 variants—most notably the one wreaking havoc on British life—is expected to further threaten the U.S.’s plodding path toward herd immunity. Already, hospital systems are once again buckling. New death records are set every day. Vaccine rollout has been maddeningly slow and pandemic fatigue rampant, as evidenced in Tuscaloosa, which may soon feel the consequences of the potential superspreader event that unfolded when Alabama fans celebrated the sixth college football national title of the Nick Saban era. Even then, the worst might still be yet to come.
“It’s like when you’re reading a thriller,” says Alessandro Vespignani, director of the Network Science Institute at Northeastern University, whose research focuses on modeling epidemics. “We have the vaccine deployed. We were seeing the light at the end of the tunnel. We can put this disease in the history books. … Then we got this twist in the plot and we say, ‘This tunnel is a little longer, and it’s a little more complicated to get to the end.’ ”
Viruses mutate all the time. This was the first point stressed by each of the eight medical experts consulted for this story. “That’s the important background, that there are tons and tons of mutations,” says Shira Doron, hospital epidemiologist at Tufts Medical Center. “And typically they don’t really change anything about the virus. They change the genetic code, but they don’t make the virus any different.
“In this case, it came to light that this one genetic variant was overtaking the others in its prevalence and incidents, particularly around London. When you see one becoming way more common than the others, you’ve got to go: What is that about?”
First detected by U.K. scientists in late September, the B117 lineage of COVID-19 has since spread to some 50 countries, including the U.S., where its presence was confirmed in 14 states through Friday. Characterized by a high number of mutations, including several in the spike proteins that the virus uses to infiltrate host cells, this variant also boasts an exponentially faster secondary attack rate. In other words: It spreads faster. “A lot of the data is pointing toward, potentially, a 40% to 50% increase in transmission,” says Kucharski. “If it is genuinely 50% higher … existing measures that were just about controlling what were circulating won’t be enough with this new variant.”
While this one variant isn’t believed to increase any one person’s risk of severe illness, it will nonetheless hurt in the aggregate, with more cases invariably overcrowding ICUs and elevating the death toll. Fortunately, scientists believe the Pfizer/BioNTech and Moderna vaccines will be effective against this variant—but whether those vaccines are distributed in time to stem further losses is another matter. “This window,” says Kucharski, “is crucial.”

So far, research has shown no indication that this variant transmits by different means than the common coronavirus (which moves largely via airborne droplets). But because government funding for the genomic testing of new mutations is minimal—“a big hole in our pandemic response,” says Doron—little is known about exactly why this one is more contagious. Or, for that matter, what it all means for the public health guidelines we’re asked to follow. “Six feet might not be enough,” says Penn State evolutionary microbiologist Andrew Read. “We don’t know.”
One thing, though, seems all but certain: Some highly contagious variant will spread widely in the U.S., and soon. “It could be a disaster,” says Doron, “because it’s coming on top of a post-holiday surge, on top of every single part of this country on an [infection] upswing, very full hospitals. … If you add anything at all, you’re tipping the health care system over the breaking point.”
And since pro sports are a microcosm of the country, it's not hard to guess what is likely in store for the likes of the NBA and NHL too. “I suspect we’ll find the variant in the systems of those sports leagues,” says Amesh Adalja, an infectious disease expert at Johns Hopkins. And that “raises the stakes. Meaning: If you have a case of the new variant on your bench, it’s more likely you’re going to get more cases.”
Until that happens, the same basic health and safety recommendations apply. “There’s no reason to think that precautions like masks, handwashing, social distancing will have any less of an impact,” says Nick Davies, another epidemiologist at the LSHTM. “It just means those procedures need to be followed a lot more stringently.”
If there are cracks in the defense, more contagious variants are likely to exploit them. Not long ago, the Celtics' Tristan Thompson and Grant Williams entered quarantine after reportedly sharing a maskless car ride with infected teammate Robert Williams. Neither player caught the virus, but next time they might not be so lucky.
“It’s a no-brainer that the outside-the-game stuff”—like talking face-to-face after a game or, say, partying without a mask, as Nets point guard Kyrie Irving was recently fined $50,000 for doing—"has to be completely out of the question,” says Doron. “If people really want to play, they should not be interacting with anybody else, ever. Go home, rest, come back for the game. But if you’re talking about a contact sport, there’s no way to eliminate that risk. Testing can decrease it. But when you’re getting within six feet of people and touching people, there’s no way.”
The potential consequences of another viral wave are acute. In the NBA, the Raptors have relocated to Tampa; in the NHL, the Sharks were forced to hold training camp in Scottsdale, Ariz. But what if regional lockdowns grow more widespread? Each of those leagues built a successful bubble before vowing not to return in 2021. How will they react if the choice is between another isolation or another suspension of play? And what is the threshold for that break-glass scenario? When is it no longer responsible to keep crisscrossing the country to play games?
For now, these leagues are soldiering ahead. “Monitoring developments but nothing more at this point,” NHL deputy commissioner Bill Daly wrote in an email. “The variant has not caused us to modify our protocols to this point.” The NBA, meanwhile, tightened its rules last week, barring guests from road hotels and limiting pregame locker room meetings to fewer than 10 minutes, among other new measures. “In ongoing consultation with the CDC and infectious disease specialists, we’re taking measures to address the continued challenges of the pandemic, including new viral strains,” emailed the league’s director of sports medicine, John DiFiori. (An NFL spokesperson pointed to a recent NFL Network appearance by chief medical officer Allen Sills, who said the league is "screening any new positive cases for the genes that would reflect one of these new variants.")
Several experts imagined constructive roles for these leagues in combating whatever comes next in this pandemic. The NBA partnered with Yale researchers on a groundbreaking saliva test during the playoffs; any of these leagues could fill a similar gap by funding genomic testing. “I wouldn’t say they have to do that, but the more people we have sequencing,” says Adalja, “the more likely we are to discover new variants and understand them.” At a minimum, experts say, athletes and team staffs must set examples for the general public—which hasn’t always been the case. Citing “concerning scenes,” a recent letter from Premier League leadership reminded teams that players are forbidden from hugging, high-fiving or swapping jerseys with opponents. “And don’t … go to a nightclub in the middle of a pandemic,” says University of Edinburgh virologist Elly Gaunt.

Maybe, if everything breaks right, sports leagues somehow muddle through this bleak winter, hanging on tight until players—and the rest of us—are finally all vaccinated. Until we reach the end of that tunnel.
“Obviously we want sports, and we want activities that provide leisure and fun,” says Vespignani. “And I understand that for professional players—especially to play in an arena where there is no audience, to stay in a bubble aside from the family—it’s difficult. But these are difficulties we’re all facing in different ways. Children do not go to school. We work from home. So we all need to cope with that for a few more months and be very strict with the rules.
“It’s like in football. We are in the red zone. You want to keep pushing. This is not the moment to think about relaxing or victory celebration. We need to cross the line.”