With no way for players to "test out" of 14-day quarantine after exposure to COVID-19—regardless of whether they ever tested positive—some in the NCAA see the need for change. Science might say otherwise.
The airplane looked half empty because it was.
The football players of this particular team were practicing social distancing while flying 30,000 feet in the air on a Delta jet en route home from a game. They had more than enough distance between them, or so it seemed. In some places, they were separated by two empty seats and others two empty rows. But a day later, when a small number of players on that flight tested positive for the coronavirus, school officials were forced, through a stringent contact-tracing process, to quarantine so many athletes they had to cancel their ensuing game.
At another school, a group of offensive linemen gathered one night to dine over pizza. Later that week, a player among the group tested positive and then the rest were sent into quarantine, wiping out enough of the offensive line that they, too, had to cancel the next scheduled game.
Coaches aren’t exempt from contact tracing, either. A group of coaches at one school, in fact, recently found themselves in a 14-day quarantine. A fellow staff member tested positive after they’d spent four hours with him in a press box booth calling a game.
Contact tracing can extend to families as well. Two players from the same team missed a crucial conference game last month after having to quarantine as high-risk contacts. Why? The daycare center in which their young children attend experienced an outbreak.
Administrators, coaches and team doctors shared these stories with Sports Illustrated under the condition of anonymity to protect privacy information.
There are plenty more. One-quarter of the way through the 2020 season, these stories are unfolding across college football, as the sport labors to hold a season amid a pandemic while adhering to protocols designed to protect the health and safety of the very same people, athletes and staff, who are frustrated by them.
As industry insiders predicted over the summer, one specific protocol has been more challenging than any other.
“The contract tracing is killing us,” says Todd Berry, executive director of the American Football Coaches Association. “All the sudden the coaches are calling me. They tell me that one kid got it and 12 are out (for contact tracing), and none of the 12 even ever had it.”
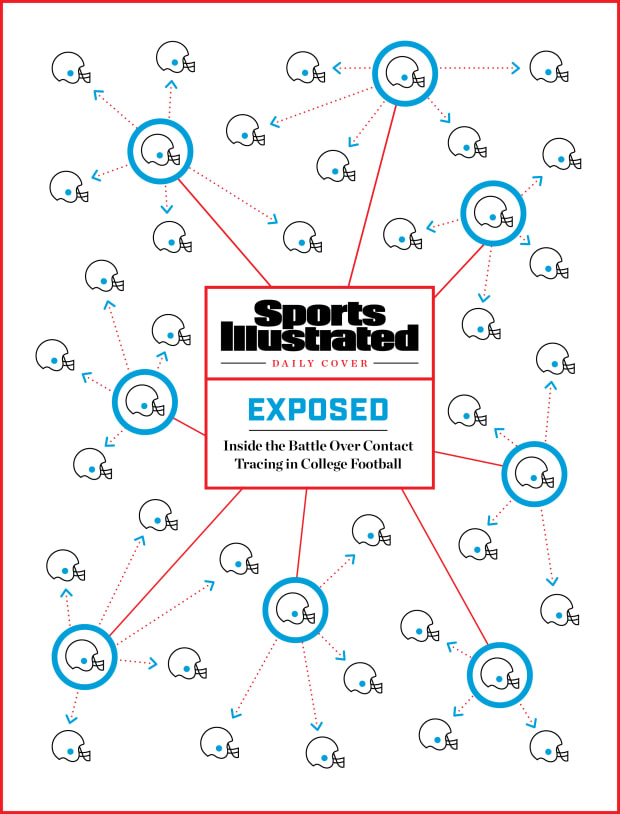
A subjective process executed differently from school to school, contact tracing has resulted in dozens, if not hundreds, of college football players missing two weeks of activity—practices, games, you name it—for having been in close contact with a positive carrier of the virus. The current operating CDC guidelines define a high-risk contact as someone within six feet of an infected person for at least 15 minutes without each party wearing a mask.
According to the CDC, and enforced by local health departments, high-risk contacts must quarantine for a mandatory 14 days.
The lengthy quarantine time is inconsistent among schools and is nine days longer than the NFL’s own protocol. The policy has created friction through the ranks of college athletics, from players to coaches and even to administrators.
In fact, high-ranking college athletic leaders have been exploring for weeks an adjustment to allow close contacts to leave quarantine inside of eight days with at least three consecutive negatives tests, a model that is most commonly referred to as “testing out,” and one the NFL operates under today.
However, a hurdle stands in the way. A spirited battle rages between colleges and conferences against local health departments over the 14-day mandatory period, the former attempting to convince the latter to approve such adjustments.
“We’ve had two athletes who have been under quarantine twice now.
Twenty-eight days taken from them, and they were never positive,” says Mack Rhoades, the athletic director at Baylor whose program is battling an outbreak of its own this week. “With health and safety as the No. 1 driver, I think there’s a better way for us to do contact tracing.”
***

Kentucky’s COVID-19 command center is located in an old seminary adjacent to the Lexington campus.
Inside what were once classrooms and dorms, more than 50 staff members bustle around while working in socially distant pods, many of them on the phone and monitoring the university’s “Health Cloud,” which tracks COVID information across UK’s campus.
The job of a contact tracer is far from easy. The process is maybe most akin to a police detective’s work in trying to crack a case, interviewing and interrogating subjects to determine who spent enough time near an infected person to be considered a close contact. They attempt to trigger memories by examining a person’s social media feed and class schedule.
“It’s labor heavy, but it’s also time sensitive,” says Lance Polston, codirector of UK’s Health Corps Project.
College campuses across the country have transformed empty or unused buildings into hubs to house their contact tracers. Some, meanwhile, are operating remotely, such as at Arkansas State, which has some 50 contact tracers and another 10 to 15 case investigators working from different on-campus offices or their homes. Case investigators normally perform the more granular aspects of evaluating potential high-risk contacts to answer important questions.
Were you within six feet for 15 minutes of a positive without a mask?
Were you around them for five minutes and then later for 11 more minutes without a mask?
Are you certain you were six feet away? And did your mask cover your nose?
Sometimes the answers they get aren’t kosher. In retelling a specific story, one team doctor said that interviews with an infected player produced zero close contacts because the athlete claimed he “always wears a mask.” The doctor conducted subsequent interviews with other players on the team who revealed the positive athlete attended a recent house party—mask-less.

“I feel like I’m juggling flaming chainsaws,” the doctor told SI, speaking under condition of anonymity.
While Kentucky’s athletic department leans on its university to assist in contact tracing, some universities are devoid of such resources. In the Sun Belt, for instance, sports team doctors and sometimes trainers are balancing their normal duties with an extra four hours a day spent tracing and testing athletes.
“In the ideal world, there would be an office somewhere that had lots of people ready to make phone calls and contact trace every positive case in America,” says Jeff Dugas, Troy’s team doctor and an orthopedic surgeon in Birmingham who chairs the Sun Belt’s COVID-19 advisory panel. “That’s not what happens.”
On average, one positive athlete often results in two-to-five close contacts who need to be quarantined for 14 days. However, as athletes and coaches improve in following COVID-19-related protocols, administrators are seeing that number continue to decrease, even dropping as low as a one-to-one ratio, says Doug Aukerman, a long time athletic physician and associate athletic director at Oregon State who chairs the Pac-12’s medical advisory board.
The more difficult number to ascertain is how many close contacts will eventually test positive during the 14-day period. One Group of Five head coach says about 40 of his athletes over the last several months have at some point been quarantined for being a close contact. Zero have tested positive. A team physician estimates her ratio at less than 10%. Meanwhile, Aukerman says that he’s unaware of any athlete testing positive in the second week of quarantine.
“By Day 7, if you haven’t turned positive, there’s a decent chance you aren’t going to test positive,” says Chris Klenck, the Tennessee team physician who leads the school’s COVID-19 program. “After Day 11, there’s almost no chance.”
The CDC’s median time for infection is about four to five days. However, its mandatory quarantine period is set at 14 days to catch those close contacts who take considerably longer to turn positive.
There are examples of close-contact patients, not necessarily athletes, who have tested negative while in quarantine on Days 5 to 9 and then produce a positive result on Day 12, says Shane Speights, the dean of the NYIT medical school at Arkansas State, who oversees virus testing at ASU.
Data and evidence is so cloudy on much of this that CDC regulations remain strict.
“People stifle about it, but that’s where the science is right now,” says Amesh Adalja, a senior scholar at John Hopkins University and an infectious disease physician who over the summer sat on the NCAA COVID-19 advisory panel.
Research, however, is ongoing. In fact, inside Kentucky’s command center, experts are conducting a project they hope to produce important results that could trigger adjustments in quarantine time. Those in quarantine agreeing to participate are tested on Days 3, 5, 7, 10 and 14.
“We want to see what conversion rate is for quarantine. How many test positive?” Polston says. “Is 14 days really the right time? At this point, the best science is telling us that.”
***

Medical experts in the college sports world say they have no evidence of on-field transmission of the virus. A dozen athletic administrators, conference commissioners, coaches and team physicians spoke to SI this week about the issue.
“I haven’t heard anybody contracting the virus in the sports environment,” says Big 12 commissioner Bob Bowlsby.
Entering the season, physicians were concerned about on-field transmission and have been actively searching for any instances. In practice and in games, they’ve seen none, according to medical personnel in the six conferences playing football. “The transmission is more intra-team,” Speights says.
The SEC has hard data to show why on-field transmission is so unlikely, says Klenck, the Tennessee doctor who sits on the SEC’s COVID-19 advisory committee. Each SEC player wears a Kinexon tracking device, about the size of a wrist watch and affixed under their shoulder pads, that measures their proximity during a game to other players. Through three games, the data is clear: Few players from opposing teams spend enough time close enough to one another over the course of a game to be considered high-risk contacts (six feet for 15 minutes).
Center and nose guards are the only ones to have logged more than 15 minutes in a game, a predictable outcome of two positions that ram against one another each play. They recorded a high in one game of 18 minutes.
Many times, it’s much lower. In fact, after Florida’s outbreak this week, Texas A&M examined tracking data from its game against the Gators last weekend. The highest cumulative time between two opposing players was six minutes, says A&M athletic director Ross Bjork.
Administrators are seeing the same in practice out west.
“The interactions are very, very short and brief,” says Aukerman, the Oregon State physician. “It takes a lot of them to meet the time requirements to meet the close-contact mark.”
However, the SEC tracking data is showing high-risk contact among players on the same team, whether it be on the sideline or in huddles, Klenck says. The goal is to avoid as many high-risk contacts as possible, both for safety and for sanity, given that 14-day mandatory quarantine time.
But as time marches on, as data is uncovered and as testing becomes more available and reliable, the quarantine time is on its way to decreasing, those in the industry say. In fact, Berry, the AFCA executive director, says he feels like the NCAA is “fairly close” to allowing athletes and staff to test out of quarantine. The topic has been discussed within every football conference in the U.S., most notably the SEC.
The most favorable proposal requires close contacts to test negative three consecutive days, Days 5 to 7 of quarantine, before granting them release on Day 8. They would then need to test negative for the next seven days to remain out of quarantine.
“That seems to be a level of precaution supported by doctors and scientists,” says Bowlsby, who is regularly on calls with some of the nation’s top epidemiologists and sports physicians.
The NFL has been granting close contacts the ability to test out of quarantine for weeks, requiring two negative tests separated by at least 24 hours. But this week, after a slew of outbreaks and game interruptions, the league made a change to its policy. It now requires a close contact to quarantine for at least five days, needing five consecutive negative tests to be released.
Speights, the Arkansas State physician, says any plan to test out of quarantine is a “bad idea.” He calls the NFL’s model a “failed plan” and contrary to CDC guidelines. Local health departments granted their NFL teams the ability to test out primarily because the league conducts daily testing with PCR methods, the gold standard in the industry.
It’s not so easy for colleges to get the same clearance. For instance, Big Ten schools are testing each day as well, but with rapid antigen tests, not the superior PCR. Administrators in the Big Ten, in negotiations with local health departments, are having problems in receiving the same clearance as those in the NFL, says an administrator in the league granted anonymity. Other leagues are having similar trouble, too. The SEC is using a PCR-only, three-times-a-week testing model. Not all of its league schools can get the approval of their health departments—or even their own presidents.
“It poses a huge challenge when a university quarantines students that have had close contact for 14 days while holding the student athletes on the same campus to a different, unproven standard,” says Tory Lindley, a longtime athletic trainer who is president of the National Athletic Trainers’ Association.
Some believe daily testing significantly lowers the need for contact tracing. The daily antigen testing administered in both the Big Ten and Pac-12 may even identify infected individuals before they become contagious, conference officials have said.
But there is still a lack of evidence to consistently support this theory, says Ben Pinsky, the medical director of clinical virology laboratory at Stanford and an expert in the COVID-19 testing industry. Couple that with the lower sensitivity of antigen tests—anywhere from 85-95% accurate—and the theory faces challenges.
“It’s a huge assumption considering what we know about the analytical sensitivity of those tests,” Pinsky says.
Antigen tests are better suited, doctors say, for testing symptomatic individuals and not daily testing of large groups. The tests tend to produce both false negatives and positives. The sensitivity on antigen tests is low enough that the SEC scrapped a plan to use them on Fridays before a game, instead administering a third PCR test on Thursdays. During trial runs in early September, the antigen tests produced too many false positives, uncovered only through a follow-up PCR test.
Testing out remains a talking point in the league, says Klenck, because of the rate in which the conference is testing. Daily testing is being discussed, too.
“I wouldn’t advocate for the general population to test out, but we test so aggressively. … There is potential we could shorten that quarantine time in a safe manner,” he says.
Testing is a tricky issue with ranges of views from conference to conference. Some can’t afford three tests per week, let alone seven. Others can’t get test results returned quick enough for daily testing.
“The NFL has unlimited resources, and the SEC too,” says Dugas, the Sun Belt medical adviser. “They can test every day. That is a huge financial burden. Without daily testing, testing out of quarantine would be tough.”
***

Mack Rhoades, the Baylor athletic director, is confident that, eventually, close contacts will be allowed to test out of quarantine. However, he believes it won’t come for at least another couple of months.
“My gut is we don’t get there by the end of football,” he says, “but potentially there’s a change that will impact basketball.”
To hold a basketball season, a testing-out model might be a necessity. While football activities don’t include enough interaction to present high-risk contacts, basketball games and practices will invariably produce close contacts, experts contend. The sport is played indoors, for one, and game or practice action involves longer stretches of close contact among players.
One positive on a basketball team could land the entire squad—and staff—in quarantine for 14 days, experts say. The only way out of it? Daily testing.
“I could see that happening,” says Bjork, “but you’ve got to ensure you’re inserting PCR tests at a high level.”
Basketball practices started this week, and the first game is scheduled for Nov. 25. The sport is producing anxiety among the medical and administrative fields. After all, how can small conferences afford a daily testing model? Without it, they risk full-team quarantine with a single positive test.
“Contact tracing will be impactful with basketball,” Aukerman says. “There is a likelihood it will involve the majority of the team.”
However, tracing is subjective in nature. There is no oversight from the NCAA or a third party to ensure programs are adhering to proper tracing standards.
Already in football, there are differences across the country that frustrate some. Florida Atlantic is battling a second outbreak in the last month, this one totaling 18 positive cases among players and another nine on the staff. In addition to those, more than 20 players are in quarantine for contact tracing.
“Every school is not the same,” says FAU head coach Willie Taggart. “It’s something you wish it was the same for everyone. It’s frustrating. You have guys testing negative, and they have to sit out 14 days. You wish there was another way.”
Shane Lyons, athletic director at West Virginia, says he’s noticed that tracing protocols are not “100% consistent” from team to team and conference to conference. Berry says he receives calls from coaches complaining that their top rival is handling the process differently and less stringent than their own.
In fact, Bowlsby says he knows of schools that are allowing athletes out of quarantine before the 14-day period. It’s a matter of the local health officials and on-campus officials to make those determinations, he says. There are different views and enforcement at institutions. “It’s the same quandary of ‘Why do some stadiums get 20% attendance and some get 30% and some don’t get any?’” Bowlsby says.
In the meantime, college football marches on amid a pandemic attempting to leap over the next hurdle. At least 30 games have been postponed or canceled for COVID-19-related reasons, something administrators expected and say isn’t alarming when “looking at the big picture,” Lyons says. “It’s less than 10% of the games.” However, that number continues to rise. After seven postponements last week, 15.8% of scheduled games have now been postponed for COVID-related reasons.
“COVID is like Las Vegas. Each time you think you’ve got it figured out, you’re wrong,” says a team physician based in the South. “COVID is the house. It always finds a way to win.”
The fight is far from over, too. Speights, the physician at Arkansas State, has his doubts. He recalls giving an interview in late June when he told a reporter that he was confident in the 2020 football season beginning.
“But,” he recalls, “ ‘I’m not convinced we’ll finish.’ My mind hasn’t really changed on that.”